Pain on the outside of the foot is known as lateral foot pain. This type of pain can be stabbing, burning, or aching. It can also be bothersome or debilitating. Severe pain can limit standing, walking, exercise, and other activities. This type of pain is not as common as other kinds of foot pain and identifying its source can be challenging. Causes of pain on the outside of the foot can include, but not be limited to, ankle sprains, arthritis, and bunionettes. Ankle sprains causing lateral foot pain are more apt to occur in those people who have high arches. Activities that cause the foot to twist, roll inward, or suddenly change directions, are common causes of ankle sprains. Arthritis causes pain and inflammation in joints. A bunionette which is also called a tailor’s bunion is a bone malformation that causes the base of the pinky toe to jut outward. If you experience pain on the outside of the foot that does not improve with rest or begins to feel worse, it is important to seek the counsel of a chiropodist who can provide you with a diagnosis and advise you of the best course of treatment.
Foot pain is a common problem treated by chiropodists. If you have foot pain, please consult with one of the specialists from Thornhill Foot Clinic. Our chiropodists can help you maintain the health of your lower limbs and your mobility.
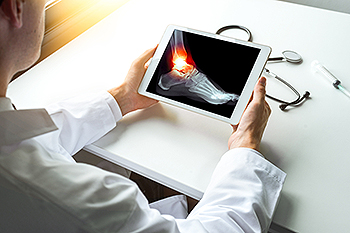
When you are experiencing foot pain, it’s important to note the type of pain and its location, as this can help determine a diagnosis.
Pain in the top of the foot may be caused by:
Stress fractures
Sinus tarsi syndrome
Extensor tendonitis
Tibialis anterior tendonitis
Gout
Athlete’s foot
Ganglion cysts
Pain in the bottom of the foot may be caused by:
Plantar fasciitis
Foot cramps
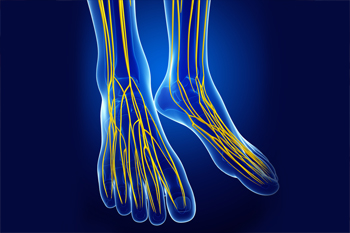
Tarsal tunnel syndrome
Plantar fibromatosis
Posterior tibial tendonitis
Stress fractures
Flat feet
Pain on the side of the foot may be caused by:
Ankle sprain
Cuboid syndrome
Peroneal tendonitis
Stress fractures
Bunions
Corns or calluses
Posterior tibial tendonitis
Heel pain may be caused by:
Plantar fasciitis
Achilles tendonitis
Bone spurs
Heel fractures
Retrocalcaneal bursitis
Sever’s disease
Pain in the toes may be caused by:
Gout
Hammertoe
Turf toe
Bunions
Ingrown toenails
Blisters
Arthritis
These and many more conditions can be treated by a chiropodist. If you have any questions, please feel free to contact our office located in . We offer the newest diagnostic and treatment technologies for all your foot care needs.