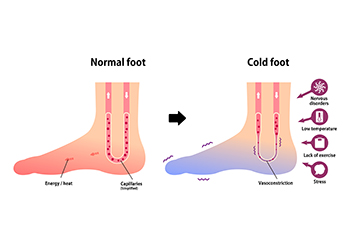
Scleroderma is a rare, chronic autoimmune disease affecting skin and internal organs. It stems from immune system-induced inflammation and tissue changes, often resulting in skin tightening and thickening. It can also affect joints, muscles, and various organs such as the heart, lungs, kidneys, blood vessels, or intestines. While predominantly affecting women aged 30 to 50, children can develop a juvenile form of scleroderma. There is no cure for this disease, however symptom management and improved quality of life are achievable through treatment. Signs and symptoms of scleroderma vary, from minor to life-threatening. One early indicator is Raynaud's phenomenon, characterized by color changes in toes due to cold exposure. Patients may experience red, white, or blue toes, along with swelling, numbness, pain, or ulcers. Other symptoms arise depending on organ involvement, requiring diagnostic assessments like blood tests, autoantibody detection, and imaging. Treatment options include medications for improving circulation in Raynaud's disease and addressing skin thickening and organ complications. Lifestyle adjustments, such as staying warm and protecting extremities, can enhance comfort. If you have scleroderma and it is causing you pain or affecting your mobility, it is strongly suggested that you make an appointment with a chiropodist for treatment that can help you live more comfortably.
Systemic diseases are medical problems that affect the entire body. Many systemic diseases can bring about foot and ankle problems. If you have a systemic disease that affects your lower limbs, please consult with one of the specialists from Thornhill Foot Clinic. Our chiropodists can help you maintain the health of your lower limbs and your mobility.
Which systemic diseases can affect the feet?
Peripheral artery disease - Causes inadequate blood flow to the lower limbs
Peripheral neuropathy - Nerve damage in the nerves that supply the feet and ankles
Diabetes - Can cause nerve damage, poor circulation, and a weakened immune system that can lead to the formation of poorly healing wounds on the feet
Arthritis - A disease of the joints that damages joint lining, it often affects the small joints of the feet and the ankle joints
Gout - A build up of uric acid in the bloodstream that forms crystals that can lodge in the joints
How can a chiropodist help?
Chiropodists help people who have systemic disease manage and maintain their foot health in a variety of ways. They can diagnose a multitude of foot and ankle problems, screen for certain systemic conditions, teach patients about proper foot care, and provide information about preventive strategies that patients could employ to avoid complications from their systemic diseases. Chiropodists can also treat foot and ankle problems through medications, foot and ankle exercises, orthotics, and lifestyle recommendations, among many other potential treatments
If you are living with a systemic illness that impacts your foot health, please feel free to contact our office located in . We offer the newest diagnostic and treatment technologies for all your foot care needs.